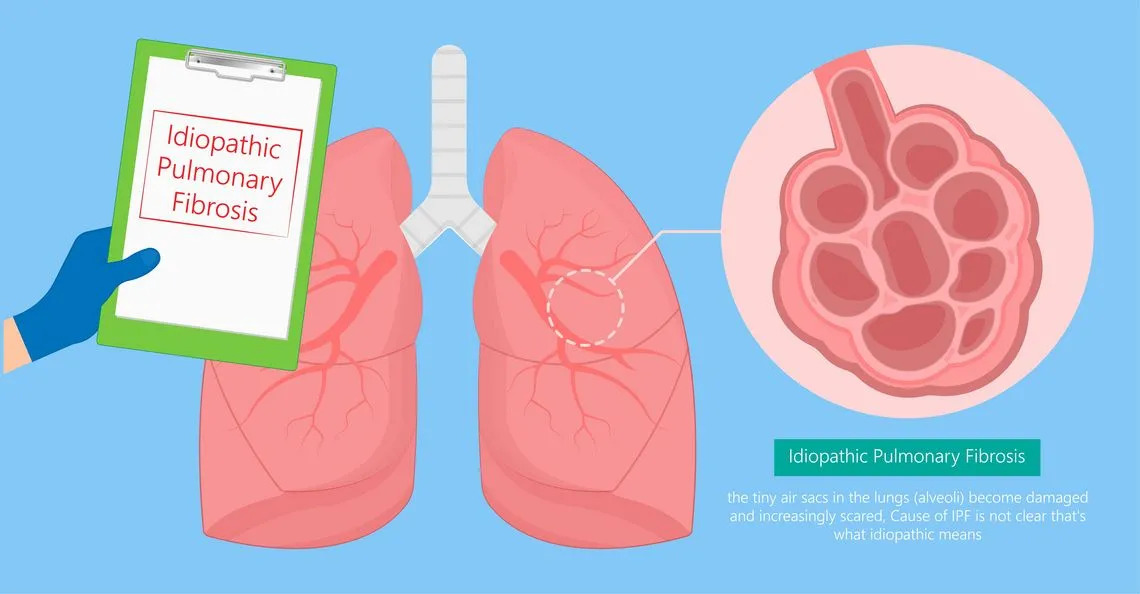
At present, the natural history of IPF is unpredictable for individual patients. To date, identification and validation of biomarkers for confirming diagnosis, assessing disease severity, prognosis, and response to treatment (theranostic markers), represents one of the main research fields in IPF1. Biomarkers discovery will contribute to unravel pathogenetic mechanisms underlying IPF development and its progression, potentially providing new therapeutic targets. Genetic alterations, especially those related to telomere coding genes, can be predictive of the likelihood of developing IPF and thus may be helpful for diagnostic purposes. Although personalized medicine is not yet established in IPF with regard to genetic alterations, in the next years could become a concrete perspective2.
Beside the standard of care represented by antifibrotic drugs, new promising are under investigation in IPF. Most of the trials target molecules involved in different fibrosing processes in the lung driven by cell populations like fibroblatsts, macrophages and lung epithelial cells. Other studies focus on the immune system, targeting lymphocytes T and B, which release mediators able to promote fibrotic processes in the early phase2.
Innovative preclinical approaches are also attempting to reverse fibrosis, but new data have to be taken with caution.
Several lines of evidence imply that in IPF progression, acute respiratory deterioration including acute exacerbation and mortality are associated with altered microbiome, i.e. the microbial community occupying the lung, with increased bacterial load or abundance of specific microorganisms. Recent data suggest that impaired microbiome is associated with inflammation, aberrant lung repair and can lead to acute exacerbation3. Targeting the microbiome, e.g. by antibiotic drugs, might be a possible therapy to slow progression of the disease.
Not least of all, ongoing clinical trials are focusing on the outcomes of pulmonary rehabilitation in IPF. Recent data support the role of pulmonary rehabilitation as an essential component of management of patients with IPF and thus is a major feature of recommendations in national and international guidelines2. Rehabilitation should include also nutritional support, education, psychological and symptom management, thus being part of a holistic approach. The research spectrum on non-pharmacological therapies in IPF is rapidly expanding and aims at improving patients’ quality of life and symptoms management, especially cough.
All these different research strategies are paving the way for a revolution in the management and treatment of this condition in the next few decades.
Francesco Bonella, Center for interstitial and rare lung diseases, University of Essen, Germany
References
- Stainer A et al. Molecular Biomarkers in Idiopathic Pulmonary Fibrosis: State of the Art and Future Directions. Int J Mol Sci. 2021.
- Somogyi V et al. The therapy of idiopathic pulmonary fibrosis: what is next? European Respiratory Review 2019
- O’Dwyer et al. Lung microbiota contribute to pulmonary inflammation and disease progression in pulmonary fibrosis. Am J Respir Crit Care Med 2019